-

Rapid Response Team Codes Following Transition-of-Care from the Emergency Department to an Inpatient Medicine Unit
Kerrin Bersani and Brett Todd
Publication Date: 5-2023
Transitions-of-care from the emergency department (ED) to an inpatient unit have been identified as a high-risk period for medical error due to multiple causes, such as communication mishaps, excessive workload, variability in patient flow, and unclear assignment of responsibility. Patients who experience a diagnostic error are also at increased risk for poor outcomes, including increased length-of-stay and mortality. Rapid Response Teams (RRTs) are frequently utilized by hospitals to address a sudden deterioration in clinical status, often after a transition-of-care. We investigated the occurrence of RRT in patients shortly after a transition-of-care from the ED to a medicine unit. Further, we analyzed the rates of RRT across various demographic groups.
-

Beyond COVID-19: The Impact of Recent Pandemics on Medical Students and their Education: A Scoping Review
Moneb Bughrara, Stephanie Swanberg, Victoria Lucia, Keaton Schmitz, Dawn Jung, and Tracy Wunderlich-Barillas
Publication Date: 5-2023
Over the past two years, COVID-19 has greatly altered undergraduate medical education (UME) as well as daily life. Medical schools across the world were disrupted and had to immediately adapt the educational experience to the online environment in order to continue the delivery of quality UME. However, COVID-19 was not the only recent pandemic. This posed the question, were similar disruptions and adaptations also seen in recent past pandemics such as Severe Acute Respiratory Syndrome (SARS) or Middle East Respiratory Syndrome (MERS) that could have prepared UME for COVID-19? This scoping review investigated the educational and personal impact of recent pandemics on UME and medical students.
-

Encephalitis: Acyclovir Toxicity or Varicella Zoster Virus?
Christine Carline, David Hess, and Diane Paratore
Publication Date: 5-4-2023
Varicella zoster virus (VZV) encephalitis can cause headache, vomiting, fever, altered mental status (AMS), ataxia, visual hallucinations and seizures1
▪ Acyclovir toxicity has similar symptoms such as hallucinations, confusion, AMS and dysphasia2 .
▪ Therefore, it can be difficult to distinguish acyclovir toxicity from VZV encephalitis.
▪We will discuss a patient with symptoms concerning for these diagnoses.
-

Purr-Ils of the Liver: A Case of Mash Cirrhosis Complicated by Disseminated Pasteurella
Joanna Henry, Alaa Abujame, Cameron Hubbard, Angela Shermetaro, James Hebden, Hussein Bazzy, Jared Grodman, Katie Sumnicht, and Christopher Cooley
Publication Date: 5-4-2023
Pasteurella Multicoda is a gram-negative coccobacillus that is commensal to mammals such as domesticated pets and transmitted to humans by scratches or bites. The extent of infection is often limited to soft tissue, bone, and joint.
Disseminated infection by P. multicoda infrequently is typically associated with peritoneal dialysis.
We present a case of disseminated P. multocida infection with bacteremia and peritonitis in a patient with NASH Cirrhosis
-

Impact of Earlier Ophthalmology Clerkships on Medical Student Match Rates in Ophthalmology
Andrew Lee and Steven Joseph
Publication Date: 5-2023
The purpose of this study is to analyze the association between earlier clerkship exposure and match success, specifically in ophthalmology. Medical schools are constantly changing their clinical curriculums to provide a stronger foundational education to their students. The structure of each medical school’s clerkship curriculum varies in timing, length and availability of certain core and elective rotations. Gaining a better understanding of the factors that affect student match rates in certain specialties can influence changes in clinical curricula to maximize future match success.
-

A Prospective Sonographic Evaluation of Peripheral Intravenous Catheter Associated Thrombophlebitis
Nicholas Mielke, Steven Johnson, Patrick Karabon, and Amit Bahl
Publication Date: 5-2023
Thrombophlebitis associated with peripheral intravenous catheters (PIVCs) is a poorly described complication in the literature. Given limited accuracy of current assessment tools and poor documentation in the medical record, the true incidence and relevance of this complication is misrepresented. We aimed to identify risk factors in the development of thrombophlebitis using an objective methodology coupling serial diagnostic ultrasound and clinical assessment.
-

Family/Decision maker Perception of Patient Care and Withdrawal of Life Sustaining Treatment
Joshua Paul, Revelle Gappy, Tracy Wunderlich-Barillas, and Robert A. Swor
Publication Date: 5-2023
Withdrawal of life sustaining treatment (WLST) is the process by which a patient has life supporting measures removed when a decision is reached that further care if futile. This process is a complex interplay of medical science, the healthcare teams’ past experiences, and communication with the patient’s family/decision maker Family members are commonly called upon to make critical decisions regarding the provision or withdrawal of patient care. Our objective was to describe the perceptions and experiences of the family members of patients who were admitted to an intensive care unit after resuscitation from an Out of Hospital Cardiac Arrest (OHCA).
-
Stress Induced Electrical Storm with Recurrent ICD Defibrillation
Joshua M. Smith and Frank Schell
Publication Date: 5-4-2023
Electrical storm is a life-threatening condition where a patient may experience frequent episodes or persistent ventricular arrythmias. With improved medical treatment of advanced heart failure patients, patients with electrical storm are presenting more commonly to emergency centers. Patients with implantable cardiac defibrillators experiencing multiple appropriate defibrillations need emergent evaluation and a systematic approach by Emergency Physicians.
-

Evaluation of online patient information regarding emergency center utilization
Rachel Truland and Steven Joseph
Publication Date: 5-2023
The decision a patient makes when seeking emergency medical care comes with risks and ambiguity if the right decision is not made. The internet is increasingly accessible to patients, and they often consult an internet search prior to seeking healthcare. The aim of this study is to assess the readability and reliability of online information regarding a patient’s decision to seek emergency care.
-
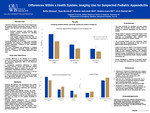
Differences within a health system: imaging use for suspected pediatric appendicitis
Nafisa Bhuiyan, Ryan Nierstedt, Michelle Jankowski, Shanna Jones, and Aveh Bastani
Publication Date: 5-2-2022
INTRODUCTION
Ultrasound (US) is the first line imaging used for suspected pediatric appendicitis. However, following equivocal US findings and its lower negative predictive value for ruling out appendicitis, Computed Tomography (CT) imaging is often performed in children. This study investigates the differences in imaging utilization between a community hospital (Beaumont Troy) and a children’s ED hospital (Beaumont Royal Oak), making it the first study to evaluate suspected pediatric appendicitis in Beaumont Health System. It also aims to further characterize differences in patient outcomes such as surgery, length of hospital stay, complications of appendicitis, and highlight the need to reduce unnecessary CT use due to its radiation exposure. -

A Case Report of a Rare COVID-19 Complication: a Subdural Empyema in a Pediatric Female
Christine Carline, Scott Klein, Christopher Cooley, and Daniel Zoller
Publication Date: 5-2022
• There have been few reported cases of intracranial complications in patients with COVID-19 and even fewer cases in children.
• A subdural empyema (SDE) is an intracranial abscess between the dura and arachnoid mater.
• A SDE usually occurs due to sinusitis, most commonly the frontal sinus, or acute otitis media
-

Evaluation of Implementing ‘Team Strategies and Tools to Enhance Performance and Patient Safety’ in a Community Emergency Department
Bryson Caskey, Shanna Jones, Sarah Berry, Heather Harris, David Donaldson, and Aveh Bastani
Publication Date: 5-2-2022
This study sought to provide an initial evaluation of implementing the program ‘Team Strategies and Tools to Enhance Performance and Patient Safety’ (TeamSTEPPS) in the William Beaumont Troy Emergency Department (ED). TeamSTEPPS integrates teamwork into medical practice by developing tools and strategies within leadership, situation monitoring, mutual support, and communication to increase team performance in order to improve quality, safety, and efficiency of healthcare1,2 (figure 1). It was implemented in the Troy Beaumont ED in 2017. This study was designed to determine if the program is achieving desired outcomes, identify areas for improvement, and add to the limited fund of data on the effectiveness of TeamSTEPPS in community ED’s3-5.
-

Journal Club in the Pre-Clinical Years During Medical School
Kristin Cuadra and Steven Joseph
Publication Date: 5-2-2022
INTRODUCTION
Traditionally, journal clubs have been conducted within graduate medical programs to help integrate evidence-based learning. This study will be focused on beginning to integrate journal club into the pre-clinical years while implementing successful techniques used in past journal clubs. Our hypothesis is that, with a structured review instrument in place to help students analyze clinical articles, students will be able to benefit from monthly journal clubs and fully grasp concepts taught in these pre-clinical years. Overall, the results will contribute significantly in determining the efficacy of journal club and whether or not it can be a valuable tool in medical education. -

Should I Stay or Should I Go: Discharging Low-risk Pulmonary Emboli from the Emergency Department
Matthew Drogowski, Radwa Koujana, Ali Abou-Alaiwi, David A. Berger, and Danielle Turner-Lawrence
Publication Date: 4-28-2022
Introduction
•Direct oral anticoagulants (DOACs) are effective treatment for pulmonary emboli (PE)1 •Increasing literature suggests the safety of discharging patients with low-risk PEs on DOACs2
-

Differences in Small Bowel Obstruction Outcomes in an Academic vs Community Hospital.
Kelly Fahey, Aveh Bastani, Shanna Jones, and Philip Kilanowski-Doroh
Publication Date: 5-2-2022
Small bowel obstruction: blockage in small intestine. Adhesions are the most common cause. Accounts for 300,000 hospitalizations in the US annually, and 20% of emergency surgical procedures in patients with abdominal pain. High morbidity and mortality. Average hospital stay of 8 days. 30-day readmission rate of 16%. In-hospital mortality rate of 3%. Costly diagnosis: more than $2 billion spent on admissions for adhesion-related disease in the United States. Clinical presentation: variable, includes abdominal pain, vomiting, constipation, nausea, and abdominal distention. Management. Operative: important if signs of ischemia, peritonitis, or strangulation. Conservative: includes bowel rest, nasogastric decompression, serial examinations, and a water-soluble contrast challenge. Majority of patients (65-80%) with SBO due to adhesions can be successfully managed with non-operative treatment. Wide institutional variation exists with respect to the decision on admitting service. Aim and Objective To understand the differences in admitting service (medicine or surgery) in patients with SBO on morbidity and length of stay in a large academic hospital vs a community hospital.
-

A Multimodal Approach to Reducing Opioid Administration in the Emergency Department
Eddie Ford, Vito Rocco, Shanna Jones, and Patrick Karabon
Publication Date: 5-2-2022
INTRODUCTION
The United States is battling a deadly epidemic against opioid abuse and misuse, which began as a result of pharmaceutical companies purposely downplaying the addictive potential of their opioid medications. In 2016, a Colorado health care system developed a groundbreaking alternative to opioids (ALTO) protocol for acute pain relief in the Emergency Department (ED). This protocol was adapted and implemented in the Beaumont Troy ED and is the focus of this current study. The primary goal of this study is to characterize the impact of the ALTO protocol on the rate of opioid and non-opioid administration in the ED for acute pain relief. -
Prehospital Use of Ketamine in the Pediatric Population
Ashima Goyal, Revelle Gappy, Remle Crowe, John Frawley, Nai-Wei Chen, and Robert Swor
Publication Date: 1-2022
-

The Current State of Diagnostic Error Education in U.S. Medical Schools
Dakota Hall, Sandra LaBlance, and Brett Todd
Publication Date: 5-2-2022
Diagnostic error has been identified by the Institute of Medicine as a major cause of patient harm. Despite recent focus on the importance of diagnostic error, little is known about how medical schools are educating future physicians, specifically, the extent to which it is taught. We aimed to investigate the current state of diagnostic error education in U.S. medical schools.
-

POCUS Refresh- Applying a Modern Pedagogy to Emergency Residency Ultrasound Education
Steven Johnson, Dorothy Christie Lakis, Jessica Kuxhause, and Amit Bahl
Publication Date: 4-28-2022
Objectives
- To investigate the impact of a modern refresh to our emergency point of care ultrasound (POCUS) curriculum on resident end of rotation exam performance and satisfaction, including both flipped classroom and targeted image review using an interactive application.
-

Pediatric COVID-19 leading to MIS-C
Pradeep Johns, Benjamin Glines, and Adam Vieder
Publication Date: 5-2022
Introduction
• SARS COV-2 infection in pediatric patients can develop into a rare condition known as multisystem inflammatory syndrome in children (MIS-C). In the United States, the incidence of MIS-C is 2 cases per 100,000 pediatric COVID cases.
• MIS-C is defined by the CDC as a Kawasaki Disease (KD) like illness with the following characteristics: - ≤ 21 years old - Fever ≥ 38° Celsius for ≥ 24 hours - Elevated inflammatory markers (ferritin, ESR, CRP, procalcitonin, d-dimer, fibrinogen, etc) - Evidence of multi-organ dysfunction ≥ 2 organ systems - Symptoms must be otherwise unattributable to an alternative diagnosis - Positive Sars-CoV-2 RT PCR, positive antigen test, or COVID exposure within 40 days of symptom onset.
• Data from a tertiary pediatric center in New York from 2020 demonstrated that 28% of all pediatric COVID-19 admissions required ICU level of care.
-

The Dark Side of Diverticulitis
Pradeep Johns and Eric McDowell
Publication Date: 5-2022
Introduction • Current guidelines, including the American Gastroenterological Association, have recommended outpatient treatment of uncomplicated diverticulitis. • CT scan for uncomplicated diverticulitis may demonstrate bowel wall thickening (70%), pericolic fat stranding (98%) without evidence of abscess, perforation, or fistula formation • Treating uncomplicated diverticulitis with outpatient oral antibiotics needs to be weighed with the patient's comorbidities, the likelihood of follow-up and signs of sepsis
-

ConstiPatED: Evaluation in the Pediatric ED – Practice Patterns and Trends Amongst Provider Types
Dharshana Krishnaprasadh, Margaret Samberg, Lara Fawaz, Sara Grant, and Margaret Menoch
Publication Date: 4-28-2022
Objectives
-The aim of this study is to describe practice trends by provider type: Pediatric Emergency Medicine (PEM) physicians, Emergency Medicine (EM) physicians, advanced practice providers (APP) and resident/fellows for evaluation and treatment of pediatric constipation.
-

Broad Strokes, Dissections in Young Folks: A Case Study
Jessica Kuxhause and Margaret Menoch
Publication Date: 4-28-2022
Objectives
- Describe incidence of CCADs causing pediatric strokes
- Classify the presenting histories, signs, and symptoms of patients with CCADs
- Identify factors delaying diagnosis of CCADs
-

The Impact of medical scribes on emergency physician diagnostic testing and diagnosis charting
Lucas Nelson and Brett R. Todd
Publication Date: 5-2-2022
INTRODUCTION
Since the widespread adoption of electronic medical records (EMRs), medical scribes have been increasingly utilized in emergency department (ED) settings to offload the documentation burden of emergency physicians (EPs). Scribes have been shown to increase EP productivity and satisfaction; however, little is known about their effects on the EP’s diagnostic process. We aimed to assess what effect, if any, scribes have on EP diagnostic test ordering and their documentation of differential diagnoses. -

Imaging for suspected pediatric appendicitis: Can ultrasound alone be trusted?
Ryan Nierstedt, Nafisa Bhuiyan, Michelle Jankowski, Lauren DeSantis, Aveh Bastani, and Shanna Jones
Publication Date: 5-2-2022
INTRODUCTION
Diagnosis of pediatric appendicitis relies on a combination of laboratory results, diagnostic imaging, and clinician judgement. However, the necessity of CT imaging has been questioned given radiation exposure. Therefore, ultrasound imaging has become a useful diagnostic tool, yet its sensitivity in identifying appendicitis is often lower in comparison to CT. This study aims to determine the sensitivity of US imaging for pediatric appendicitis and if differences exist in the diagnosis of appendicitis utilizing both CT and ultrasound or ultrasound alone.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.

