-

Influence of Medicaid and Medicare on Total Joint Arthroplasty Outcomes: 10-year Report of Michigan Hospitals
Madeleine DeClercq, Jacob Keeley, Robert Runner, Kevin Weisz, Leonardo Cavinatto, and Drew Moore
Publication Date: 5-2025
Access to healthcare significantly varies by medical insurance type, particularly for individuals for low socioeconomic status.
• Medicaid often covers these individuals (a government-funded program for low-income adults and children).
• Only 45% of primary care providers accept new Medicaid patients, versus 94% for private insurance.1
• Large non-profit medical centers accept Medicaid but still present considerable access challenges for patients.
• Lower reimbursement rates, complex medical needs, and extensive administrative requirements are key barriers for providers accepting Medicaid.
• Studies, such as those by Deans et al., highlight greater travel burdens for Medicaid patients needing revision hip or knee arthroplasty.2
• Medicaid patients often receive care in facilities where surgeries are performed less frequently, correlating with poorer outcomes.3
• Medicare primarily serves the over-65 demographic, those with disabilities, and end-stage renal disease patients à a significant portion of orthopedic cases
• Better access than Medicaid but challenged by declining reimbursements.
Purpose
• To elucidate the impact of insurance type—Medicaid, Medicare, and private insurance—on short-term outcomes, complications, and patient reported outcomes (PRO’s) following total joint arthroplasty over a tenyear period.
Hypothesis • Individuals with Medicaid or Medicare are hypothesized to experience higher complication rates and inferior PROs compared to those with private insurance
-

Gender and Racial Disparities in Pediatric Orthopaedic Surgery Fellows: A Decade-Long Analysis
Naomi Haque, Mazen Zamzam, Imran Bitar, and Ehab Saleh
Publication Date: 5-2025
- The Association of American Medical Colleges (AAMC) has highlighted the increasing gender, racial, and ethnic diversity among medical student applicants, noting a significant rise in the number of underrepresented students.
- In the 2021-2022 academic year, there was an 18% increase in total applicants. The number of Black or African American applicants rose by 21%, with Black or African American students comprising 11.3% of matriculants in 2021, up from 9.5% the previous year. First-year students of Hispanic, Latino, or Spanish origin saw a 7.1% increase, making up 12.7% of matriculants. Additionally, women constituted 56.8% of applicants, 55.5% of matriculants, and 52.7% of total medical school enrollment.1
- Despite these positive trends in medical education, the field of orthopedic trauma surgery has not experienced similar diversity advancements. The number of applicants to orthopedic surgery residency programs has remained relatively constant, but there has been limited examination of the demographics of orthopedic trauma fellows.
- A review of orthopedic surgery programs revealed that while there is an incremental increase in the number of female and underrepresented minority residents, the fellowship programs, specifically in orthopedic trauma surgery, lag in this diversity.2 Furthermore, orthopedics’ slow increase in female residents lags behind that of other specialties.3 A survey conducted by the American Academy of Orthopedic Surgeons (AAOS) in 2008 revealed that only approximately 4% of orthopedic surgeons responding to the survey are female.4
-

Second-Site Periprosthetic Joint Infection After Subsequent Primary Hip or Knee Arthroplasty
Daniel Nikolaidis, Devin Young, Andrew Steffensmeier, Robert Runner, and Mark Karadsheh
Publication Date: 5-2025
Periprosthetic joint infections (PJI) can arise anytime in the lifetime of a patient. Therefore, patients who have multiple prosthetic joints are at risk for developing multiple PJIs. Polyarticular PJI can be classified as either synchronous or metachronous. Synchronous PJIs present simultaneously in two or more joints. Metachronous PJIs (MPJI) occur in two or more joints after a disease-free period. Incidence of MPJI varies in the literature from 8-20%.1
Known risk factors associated with MPJI include Rheumatoid Arthritis, sepsis or SIRS, infection with MRSA, ≥3 revision arthroplasties, longer length of stay in the hospital, and an index TKA PJI.2
Only a few studies specifically investigate MPJI in subsequent primary arthroplasties. These studies suggest that patients who have a history of treated PJI are at an increased risk of developing a MPJI in a second arthroplasty site.3-5
-

A Review of Risk Factors for Postoperative Failure after Isolated Primary Medial Patellofemoral Ligament Reconstruction
Bilal Tarar, Ameen Suhrawardy, Clark Yin, Leonardo Cavinatto, Elizabeth Dennis, Jeffrey Fischgrund, and Betina B. Hinckel
Publication Date: 5-2025
• Medial patellofemoral ligament reconstruction (MPFL-R) is a surgical treatment for patellar instability [1].
• Cases of post-operative recurrent dislocation and persistent instability may occur due to preexisting anatomic risk factors and technical errors in the procedure.
• Current rates of recurrent dislocation are reported to be up to 20% [2].
• Research Question: What anatomic and technical risk factors are associated with increased rates of recurrent dislocation after primary MPFL-R?
-

The Effect of COVID-19 on Total Joint Arthroplasty
Hailey Worstman, James E. Feng, Alex Miller, and Drew Moore
Publication Date: 5-2025
• Arthritis is debilitating disease that is common throughout the U.S. For patients with refractory disease, total hip and knee arthroplasty, collectively known as total joint arthroplasty, are used for definitive management.1 •
Total joint arthroplasty, TJA, is one of the most common procedures in the U.S. and is typically inpatient in order to start physical therapy and promote joint mobility as soon as possible.
• Elective procedures, including total joint arthroplasties, were halted in March 2020 due to the pandemic.2,3
• When TJAs resumed they shifted towards outpatient procedures and at home physical therapy.4
• The impact of the COVID-19 pandemic on surgical outcomes is unknown for total joint arthroplasties.
-

Metachronous Periprosthetic Joint Infection in Patients with Multiple Arthroplasties at Index Infection
Devin Young, Daniel Nikolaidis, Andrew Steffensmeier, Robert Runner, and Mark Karadsheh
Publication Date: 5-2025
Periprosthetic joint infection (PJI) is a devastating complication of one of the most successful surgeries in medicine. About 1% to 2% of patients will develop PJI after primary total hip arthroplasty (THA) or primary total knee arthroplasty (TKA) [1]. The 5-year patient survival rate of THA PJI is estimated to be worse than that of common cancers, such as breast cancer [2]. The burden of this disease is likely to increase exponentially as the population ages and the number of patients undergoing total joint arthroplasties increases in the future [3].
Most devastating is what Murray et al deem as metachronous periprosthetic joint infection (MPJI) in which patients are surgically treated for an initial PJI and then develop a subsequent PJI at a second site [4]. The incidence of MPJI has been estimated to be between 6.3% and 20% [5-6]. There has been a discordance in the risk factors for MPJI, as reported in several existing studies. Most evidence has supported rheumatoid arthritis, sepsis or systemic inflammatory response syndrome at the time of initial PJI, MRSA-positive intraoperative cultures, more than 3 stages of resection arthroplasty, longer length of hospitalization, and an index knee prosthesis as the likely risk factors.
-

Quantifying the Importance of Orthopaedic Surgeon Attributes by the Public
Rasheed Abdullah, James E. Feng, Phillip Vartanyan, Hassan Alosh, Drew Moore, Leonardo M. Cavinatto, and Betina Hinckel
Publication Date: 5-2024
Evaluate what surgeon attributes are currently important to our patients, and what modalities may be most effective in finding orthopaedic surgeons, using online crowdsourcing.
-

Operative Versus Non-Operative Treatment of Z-Type Clavicle Shaft Fracture in Adolescents: A Retrospective Study
Sami Azeroual, Colin Van Wagoner, Jeffrey Leider, and Ehab Saleh
Publication Date: 5-2024
- The clavicle is one of the most fractured bones in the human body.
- Traditional treatment involves conservative management with a sling or immobilization but recently the effectiveness of the approach has been questioned.
- Studies done on the adult population have found higher rates of mal or non-union than previously noted, especially in those with displaced or comminuted fractures.
- The noted malunion or non-union was noted to have effects on shoulder mechanics, pain with overhead activity, and loss of strength and endurance.
- Due to differences in physiology the findings in the adult studies do not necessarily translate to the pediatric population.
- A Z-type fracture occurs when a middle-comminuted fracture fragment is oriented vertically and gives the fractured clavicle a Z shape.
- Some studies have recommended that these types of fractures should be treated surgically due to concerns about healing while others suggest that there is no benefit to operative treatment.
-

More Than You Can Swallow: Mycotic Aneurysm, An Uncommon Etiology of Dyspepsia
Hussein Bazzy, Katharine Glover, Steven Jones, James Aldridge, Michael Potes, and Katie Sumnicht
Publication Date: 5-9-2024
Dyspepsia is defined as predominant epigastric pain lasting greater than one month.
Common etiologies of dyspepsia include peptic ulcer disease, medications, and gastroesophageal reflux.
We present a rare case of dyspepsia caused by a mycotic aneurysm due to accidental foreign body ingestion leading to emergent inpatient intervention.
-
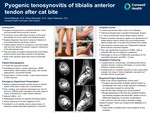
Pyogenic Tenosynovitis of Tibialis Anterior Tendon After Cat Bite
Daniel Blascak, David Sosnoski, and Aaron Seidman
Publication Date: 5-9-2024
Pyogenic tenosynovitis is a bacterial infection of the synovial sheath that surrounds a tendon.
Commonly occurs within flexor tendons of the hand; theoretically can occur within any sheathed tendon.
Delayed diagnosis may lead to spread of infection to surrounding tissues and tendon rupture.
Tibialis anterior tendon is encased in a synovial sheath that runs from above the superior extensor retinaculum to the talonavicular joint.
Only five cases of pyogenic tenosynovitis of the tibialis anterior tendon have been reported in the literature.
None of the reported cases were due to animal bite injury.
-

Comparing the outcomes of titanium and stainless steel flexible nails in repairing pediatric long bone fractures
Novelpreet Boparai, Suzan Kamel-ElSayed, and Ehab Saleh
Publication Date: 5-2024
- Traditionally, pediatric femoral fracture treatment favored conservative methods.
- Surgical intervention was deferred until age 6, as non-operative approaches often resulted in complications.
- Titanium elastic nailing (TENS) emerged as an effective treatment for diaphyseal femoral fractures in ages 6 to 16. However, the choice between TENS and stainless steel elastic nailing (SSENS) remains debated due to inconsistent findings.
-

Outcomes of Primary ACL Repair for Proximal Tears: A Systematic Review and Meta Analysis
Collin Braithwaite, Tanner Hafen, Robert Dean, Joseph Guettler, and James Bicos
Publication Date: 5-2024
The purpose of this study was to determine which primary ACL repair technique resulted in the lowest failure rates postoperatively.
-

Public Perception of Robotic Assisted Total Hip Replacement Surgery
Marvee Espiritu, James E. Feng, Phillip Vartanyan, Drew Moore, Robert Moore, and Mark Karadsheh
Publication Date: 5-2024
- Robotic or technology assisted THA has received significant attention recently due to its precision in acetabular cup placement within the Lewinnek safe zone.1
- Few studies have assessed the public’s perception of robotic-assisted THA.3,4 Insight into patients’ perception of robotic-assisted THA may yield valuable information that may impact further integration of the technology within hospitals and surgeon training.
-

Morbidity of Tendon Harvest Site for ACL Autograft; A Systematic Review
Jessi Fore, Betina Hinckel, and Elijah Auch
Publication Date: 5-2024
Primary anterior cruciate ligament (ACL) ruptures are highly common and lead to a significant number of primary ACL reconstruction surgeries in the U.S.1. When choosing a graft, surgeons can pick between auto- and allografts2. An autograft can include a bone-patellar tendon-bone (BPTB) graft, a hamstrings tendon (HT) graft, or a quadriceps tendon (QT) graft2. Currently, there is a wide range of research on graft types, but no paper compares all threes graft types directly. This review will compare literature to determine the morbidity associated with each graft type and determine which autograft is best for primary reconstruction.
-

Metastatic Osteosarcoma Involving the Skin: A Systematic Review of Patient Demographics, Clinical Characteristics, and Treatment Outcomes
Sarah Fried, Ameen Suhrawardy, Rafey Rehman, Malik Al-Jamal, Drew Moore, and Darius Mehregan
Publication Date: 5-2024
Skeletal osteosarcomas - most common primary malignant bone tumor1 and commonly metastasize to:
• Lungs (95%)2 •
Other bones (50%)2 •
Kidneys (12%)2 •
Rarely to the skin3
Extraskeletal osteosarcomas (ESOS) – soft tissue tumors that may also metastasize to the skin4,5,6
Value in gathering data on this rare phenomenon:
• Informs biology and dermatologic care of patients suffering from this cancer.
This systematic review characterizes metastatic osteosarcomas involving the skin.
-

Out of Room – International Custom 3D Printed Implant for Rheumatologic Glenoid Deficiency: A Case Report
Brian Golasa, Josiah Valk, Jared Lutsic, Justin Rebock, and Mohamed Saad
Publication Date: 5-9-2024
- The advent of 3-Dimensional (3D) printing has provided orthopaedic surgeons the ability to design custom, patient-specific implants for a variety of different complex problems notably, severe bone loss.
- Rheumatoid arthritis (RA) is a debilitating, inflammatory, systemic disease affecting approximately 1.3 million adults in the United States (US).1 Orthopaedic manifestations are plentiful. Issues unique to the shoulder are: central glenoid wear, periarticular erosions and osteopenia, and subchondral cysts. Disease modifying antirheumatic drugs can be preventative but do not restore the erosive articular damage already done.
- Glenosphere fixation is critical for reverse total shoulder arthroplasty (rTSA) implant stability and longevity. Diminished bone quality and quantity are seen in RA compromising fixation. Custom implants can allow for screw fixation into the coracoid when the glenoid vault is inadequate.
-

Assessing Patient Preferences for Technology-Assisted versus Traditional Total Knee Arthroplasty Using a Validated Online Survey Marketplace: Before and After Patient Education
Tanner J. Hafen, James E. Feng, Phillip Vartanyan, Drew Moore, and Robert Runner
Publication Date: 5-2024
- Computer (CA) and robotic (RA) assisted TKA has becoming increasingly prevalent in orthopaedic surgery1,2.
- There is limited insight into the public perception of CA and RA3.
-

Pseudoaneurysm Development After Short Cephalomedullary Femoral Nailing
Nicholas E. Runge and Daniel P. McCall
Publication Date: 5-9-2024
Hip fractures are amongst the most treated conditions by orthopaedic surgeons1 and are routinely treated with cephalomedullary nails (CMN)s.
Pseudoaneurysm formation is a rare complication after femoral CMN. The primary cause of pseudoaneurysm formation in previous studies has been found to be related to overpenetration of the far cortex with a drill or screw.
Patients with neuromuscular diseases may have aberrant anatomy potentially leading to increased risk of pseudoaneurysm formation
This the first case report of a patient with post-polio syndrome who developed a symptomatic deep femoral artery pseudoaneurysm status post short CMN fixation for a basicervical femoral neck fracture (FNF). Here we describe the work up and management of this uncommon complication.
-

Subclinical Presentation of Cutibacterium Acnes Infection Following Revision Rotator Cuff Repair: A Case Report
Zachary Walker, David Shuster, David Sosnoski, Ali Hamade, Hussein Saad, and Marc Milia
Publication Date: 5-9-2024
Cutibacterium acnes is a gram-positive anaerobic bacillus which is commonly found in the sebaceous glands of the skin generally in the axilla, chest and back regions 1,2.
Shoulder infections have been reported to occur at 3.4% following arthroscopic or open shoulder surgeries, where they are most commonly due to C. acnes3,4.
This case report demonstrates a unique case and management of a subclinical presentation of confirmed C. acnes infection.
-

Remove the Ring: A Quality Improvement Initiative for Upper Extremity Trauma
Brandon Wallace, Matthew Charlick, Josiah Valk, and Aaron Seidman
Publication Date: 5-9-2024
Upper extremity trauma is a common injury and post traumatic edema is an expected sequela. Retained rings on the digits prohibit circumferential swelling and may lead to tourniquet syndrome if left in place leading to a devastating and avoidable consequence.
Expeditious ring removal in upper extremity trauma is prudent for patient safety.
Radiographs are typically obtained early in the triage and treatment of patients suffering from upper extremity trauma. This presented itself as as reliable efficient target to have rings removed prior to this treatment step.
An opportunity to make a systemic change to maximize patient safety and care was identified with efforts made to reduce time from presentation to ring removal.
The authors proposed a hard-stop protocol. The aim was to foster interdisciplinary communication and to improve patient safety and outcomes by promoting early ring removal in the traumatic setting and thus limiting potential for this devastating complication.
-

Polymicrobial Prosthetic Joint Infection Including Mycobacterium Tuberculosis: A Case Report
Hernan Andres Yunis, Zachary J. Walker, Matthew E. Charlick, Daniel P. McCall, and Hind Hadid
Publication Date: 5-9-2024
Usual culprits of PJI affecting total hip and knee arthroplasty are Staphylococcus aureus and streptococcus epidermidis in the acute phase.
During the chronic presentation, microbes become much more diverse as they may seed due to hematogenous spread from other body sites.
The purpose of this case study was to illustrate an instance when polymicrobial total hip arthroplasty PJI included Mycobacterium Tuberculosis.
-

The Routine Use and Cost Analysis of Acid-Fast Bacilli and Fungal Cultures in Foot and Ankle Surgery: A Retrospective Study
Margaret Bohr, Robert Dean, Zein El-Zein, Megan Audet, Paul Fortin, and Zachary Vaupel
Publication Date: 5-2023
Infection is a significant complication seen in orthopaedic surgery. In such cases, samples are sent to be cultured for aerobes, anaerobes, acid-fast bacilli (AFB) and fungi. AFB and fungi are generally slow-growing, difficult to culture, and rarely the pathogen, whereas aerobic and anaerobic cultures are routinely positive and guide antibiotic treatment. The goal of this study is to evaluate the value of routinely ordering AFB and fungal cultures in the setting of foot and ankle surgery.
-

Surveillance of Dual-Mobility Hip Systems: Damage Mode and Clinical Data Analysis
Camilla Cascardo, Conner D. Ahlgren, Michael J. Maxwell, Tyler Vovos, Mark Karadsheh, and Drew Moore
Publication Date: 5-2023
Hip instability following total hip arthroplasty (THA) is a prominent indication for revision surgery. Dual mobility (DM) implants are designed to increase stability, and trending use makes characterizing in vivo damage and clinical failure modes important. This study expounds upon micro- and macroscopic damage mode findings of Lombardo et al., including novel screw ring damage using an updated retrieval registry.
-
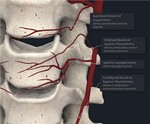
A MSSIC Study Reveals Non- Modifiable Risk Factors Were Associated with Post-Operative Hematoma following ACDF
Richard Easton, Matthew Lipphardt, Matthew Easton, Nicholas Papakonstantinou, Lonni Schultz, Hsueh-Han Yeh, and Cecile Pestano
Publication Date: 11-29-2023
Introduction
Post-operative hematoma (POH) following anterior cervical discectomy (ACDF) is uncommon . Although rare, POH is recognized as a potentially catastrophic post-operative complication . There is limited information as to who is vulnerable . From a large database, the authors sought to identify common modifiable and non-modifiable risk factors for developing POH and its associated clinical outcomes.
Materials and Methods
The Michigan Spine Surgery Improvement Collaborative (MSSIC) is a statewide quality improvement initiative . ACDF cases in MSSIC registry from 2014-2018 were identified . Patients who developed POH (POH) were compared to those who did not (non-POH) . Chi-square and t-test analyses were done to compare the two groups in terms of demographics, surgical characteristics, patient reported outcomes (baseline and postoperative PROMIS-PF score), and other postoperative symptoms or complications . All analyses were performed by using SAS 9 .4
Results
Incidence of POH is low . Of the 9,958 cases, it only occurred in 114 cases (1 .1%) . POH was associated with male gender (1 .6% vs 0 .7%, p < .001), advanced age (age 59±11 vs 55±11, p < .001), baseline use of anticoagulation (2 .3% vs 1 .1%, p= .031), previous spine surgery (1 .6% vs 0 .9%, p= .005) and inpatient procedures (1 .3% vs 0 .7%, p= .024) . POH was also associated with which cervical levels were operated (p< .001), with the highest rates observed in surgeries involving C3-C6 (3 .6%) and C3-C5 (3 .8%) while the lowest in surgeries involving C5 to C7 (0 .5%) . Smoking, multi-level surgery, corpectomy and drain use were not associated with hematoma (p> .10 for all) . Reports of dysphagia (6 .9% vs 29 .8%, p < .001), prolonged hoarseness (2 .4% vs 9 .7%, p < .001) and weakness (5% vs 10 .5%, p= .007) were common in the POH group . No significant differences in PROMIS outcomes were observed between POH and the non-POH groups at baseline (p= .232) and post-operatively at 90 days, 1 year, and 2 years (p> .05)
Conclusion
POH is rare . Intrinsic or non-modifiable risk factors identified were gender, age, baseline use of anticoagulation, prior surgery and anatomical exposure . Dysphagia, prolonged hoarseness and weakness were common in the POH group . Discussion: Although intrinsic factors cannot be eliminated, surgical risk factors can be minimized . Our large database review revealed procedures involving C3-C5 and C3-C6 had the highest rate of hematoma compared to more caudal surgeries . Difficulties with exposure as well as vascular anatomy in the upper cervical spine, the cricothyroid arteries bilaterally (Figure 1), could explain this finding . Thorough visual inspection to ensure hemostasis is obtained prior to closure is critical . POH, if left unrecognized put patients at significant risk for this life-threatening postoperative complication . Effective screening targeted at high-risk patients may help in prevention and early detection
-
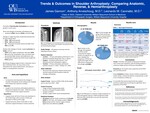
Trends & Outcomes in Shoulder Arthroplasty: Comparing Anatomic, Reverse, & Hemiarthroplasty
James Gannon, Anthony Arveschoug, and Leonardo M. Cavinatto
Publication Date: 5-2023
The field of shoulder replacement has evolved greatly since the inception of the reverse shoulder arthroplasty (RTSA) in 2004. With yearly gains of 32%, the RTSA now encompasses the largest portion of shoulder arthroplasty procedures. In contrast, the anatomic total shoulder arthroplasty (ATSA) and hemiarthroplasty (HA) have steadied or decreased. Surgical outcomes between these three procedures are mixed however. The purpose of this study was to characterize trends and outcomes between the RTSA, ATSA, and HA at a large-volume, single-institution center
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.

