-

Evaluating the Accuracy and Quality of the Information on Pulmonary Rehabilitation Videos Shared on YouTube amidst the COVID-19 pandemic
Payaum Fotovat-Ahmadi, Bilal M. Ali, and Bhavinkumar Dalal
Publication Date: 5-2023
YouTube is a visual library that is growing at incredible pace, especially with the rise of COVID-19 pandemic. Pulmonary rehabilitation refers to the rehabilitation treatment of patients with chronic pulmonary diseases. YouTube has made it possible to practice remote rehabilitation, the effectiveness of which have been proven non-inferior to traditional approaches.
-
A Survey of Medical Student Experiences During the COVID-19 Pandemic
Stephanie Gappy, Girish Nair, and Dwayne Baxa
Publication Date: 5-2023
During the COVID-19 pandemic, medical students switched from an in-person to virtual curriculum. This shift placed stress on medical schools to find alternatives to train students. Students relied on recorded lectures, emails, and video-conferencing to stay up-to-date with schoolwork. Understanding student experiences during the pandemic will help prepare students and administrators for repeat lockdown events. The goal of this study is to understand the experiences of medical students during the pandemic.
-

Impact of Structured Reporting Template on the Quality of HRCT Radiology Reports for Interstitial Lung Disease
Han G. Ngo, Girish B. Nair, and Sayf Al-Katib
Publication Date: 5-2023
This QI study compared the completeness of HRCT radiology reports before and after the implementation of a disease-specific structured reporting template for suspected cases of interstitial lung disease (ILD).
-

Evaluation of Phenobarbital in the Treatment of Alcohol Withdrawal in the Intensive Care Unit
Sienna J. Ringgenberg and Vishal K. Patel
Publication Date: 5-2023
Alcohol withdrawal syndrome (AWS) is typically managed using the Clinical Institute Withdrawal Assessment (CIWA) protocol which includes benzodiazepines, supportive care, and close clinical monitoring. Alternatives to benzodiazepines such as phenobarbital provide several advantages including less frequent dosing, longer tapering off of doses, and additional glutamate inhibition. The purpose of this study is to evaluate the effectiveness and potential benefit to using phenobarbital in addition to CIWA protocol in the treatment of AWS at Beaumont, Royal Oak.
-

Transition of continuous intravenous epoprostenol to oral treprostinil in a patient with pulmonary arterial hypertension: A patient case report
Tania Saeed, Heidi Klotz, Klea Noskey, Jacqueline Brewer, Samuel Allen, and Rebecca Baker
Publication Date: 9-28-2023
-
A Study to Compare Baseline Functional Residual Capacity and Forced Vital Capacity as Predictors of Mortality and Hospitalization in a Cohort of Mild to Moderate Interstitial Lung Disease
Olga R. Gomez Rojas, Ehsun Naeem, Filip Ionescu, Edward Castillo, and Girish B. Nair
Publication Date: 5-2022
Forced Vital Capacity (FVC) is a common parameter used to assess disease progression in patients with Interstitial lung disease (ILD) and acts as a surrogate for mortality. Previous studies suggest Functional Residual Capacity (FRC) may be an earlier predictor of disease progression in ILD. In this study, we compared predictive ability of baseline FRC to FVC to predict one-year-mortality and respiratory related hospitalization in patients with mild to moderate ILD
-
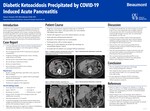
Diabetic Ketoacidosis Precipitated by COVID-19 Induced Acute Pancreatitis
Tamera Tennant and Bhavinkuma Dalal
Publication Date: 5-13-2022
Gastrointestinal manifestations of COVID-19 infection are increasingly being recognized, such as nausea, vomiting, and diarrhea. Research into the pathophysiology is ongoing. I present a case of a 52-year-old female without a history of diabetes who presented to the emergency room with progressive lethargy and altered mental status. Her tests results were consistent with diabetic ketoacidosis with glycemia 1440 mg/dL, venous pH 7.23, beta hydroxybutyrate of 7.53 mmol/L, bicarbonate 14 mmol/L, and anion gap 32. COVID-19 (SARSCoV- 2) testing by nucleic acid amplification was positive on admission. She was admitted to the intensive care unit and started on an insulin drip. Her severe abdominal pain led to the diagnosis of acute pancreatitis with lipase >1200 U/L and computed tomography of the abdomen showed inflammatory changes around the head of the pancreas and second portion of the duodenum. Workup for the cause of her pancreatitis was unrevealing. A right upper quadrant ultrasound negative for evidence of cholelithiasis, common bile duct dilation or liver abnormalities. She denied alcohol and drug use, which was confirmed with a negative blood alcohol level and urine drug screen on admission. Furthermore, she was not taking any medications prior to arrival, specifically those known to cause pancreatitis. She was diagnosed with diabetes mellitus during this admission and DKA was the presenting situation precipitated by COVID-19 pancreatitis. She was treated with intravenous fluids and supportive care. The remainder of her hospital stay was unremarkable. She was discharged home with an insulin regimen, and her HbA1C two months later was 8.3%. Follow-up CT of the abdomen one month after discharge showed no abnormalities. Literature review revealed a study in China reported an elevated incidence of pancreatic injury with few exhibiting hyperglycemia, and without a diagnosis of acute pancreatitis (1). There are few cases of acute pancreatitis that are classified as being caused by COVID-19 infection (2). However, none of these reported a complication of DKA. This case demonstrates pancreatitis and DKA as rare, yet possible, complications of COVID-19 and emphasizes the importance of thorough history-taking and diagnostic evaluation.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.

